Eviset Contributes Public Comment to the National Medically Tailored Meal (MTM) Sustainability Blueprint
Today, Eviset had the opportunity to contribute public comments to a major national policy effort—the Medically Tailored Meal (MTM) Sustainability Blueprint, developed by the Food Is Medicine Coalition (FIMC) and the Center for Health Law and Policy Innovation (CHLPI) at Harvard Law School.
The Blueprint represents an important milestone in advancing Food Is Medicine programs from pilots and grants to sustainable, reimbursable care. It thoughtfully defines a legal and operational framework for quality standardization, credentialing, and coverage—topics that closely align with Eviset’s mission to strengthen transparency and quality across social care delivery by leveraging data at scale.
Our comments emphasize how patient experience and engagement data can serve as a critical, feasible, and scientifically validated component of MTM quality measurement—reinforcing the priorities outlined by FIMC and CHLPI around standardization and long-term sustainability.
Below is the full text of Eviset’s submitted public comment.
Public Comment in Response to the The Medically Tailored Meal Sustainability Blueprint
As a data solutions company, Eviset delivers unprecedented visibility into the social care sector. Through innovative technology and a commitment to turnkey data-driven solutions, Eviset can equip medically tailored meal (MTMs) providers, managed care plans, healthcare systems, and government partners with actionable intelligence on patient experience and engagement.
Eviset appreciates the opportunity to comment on the Medically Tailored Meal (MTM) Sustainability Blueprint and commends the Food Is Medicine Coalition (FIMC) and the Center for Health Law and Policy Innovation (CHLPI) for publishing this important and timely resource. The Blueprint addresses a central challenge facing the Food Is Medicine (FIM) field: the lack of quality standardization that has limited the transition of FIM interventions from pilot and grant-funded programs to sustainable healthcare reimbursement models.
As the Blueprint notes, stakeholders have long faced barriers in defining coverage requirements, credentialing providers, and appropriately pricing services. This has resulted in wide variation in service and provider quality, inefficiencies in implementation, and missed opportunities to build a cohesive, evidence-based standard for MTMs. By grounding the Blueprint in a legal framework, FIMC has created a foundation for standardization, sustainability, and long-term integration of FIM services into healthcare systems.
The Blueprint rightly highlights the importance of designing MTM programs and evaluation frameworks that can measure, model, and predict financial impact. We wish to support the Blueprint by providing additional input regarding the critical role of patient engagement on health outcomes and cost savings. In addition, we wish to confirm that there is a feasible, affordable, and practicable method for measuring and assessing patient experience and engagement for MTM. This method addresses a broad continuum of engagement, from satisfaction and usage patterns to prevention of fraud and abuse. A scientifically valid measure set around patient experience and engagement is a mandatory input to evaluation frameworks that measure, model, and predict financial impact assessment. To put it simply, if participants are not actually consuming the meals provided, how can program performance or return on investment be accurately evaluated?
Eviset’s Client Experience Solution was developed to fill a critical data gap: the absence of patient experience and engagement information that can demonstrate how interventions create impact. Our platform captures and analyzes data at scale using science-backed questions and AI-enabled analytics, providing real-time insights that strengthen program delivery and support measurement, modeling and prediction of financial impact by providing on the ground intelligence inside people’s homes about the actual uptake of MTM interventions. Emerging evidence has shown that patient engagement data offers predictive value for health improvement. Eviset’s initial deployments have routinely seen response rates of 30% and capture data from diverse populations.
Our ability to capture patient engagement data at scale also enables critical sector guidance. Viewed in aggregate, these data can elevate factors that distinguish successful providers and programs. For example, are the highest levels of participation and health improvement most correlated with trust of providers? cultural fit of food? service personnel? or other aspects of program design? With advanced data tools like Eviset’s, these specific strengths can be illuminated and scaled.
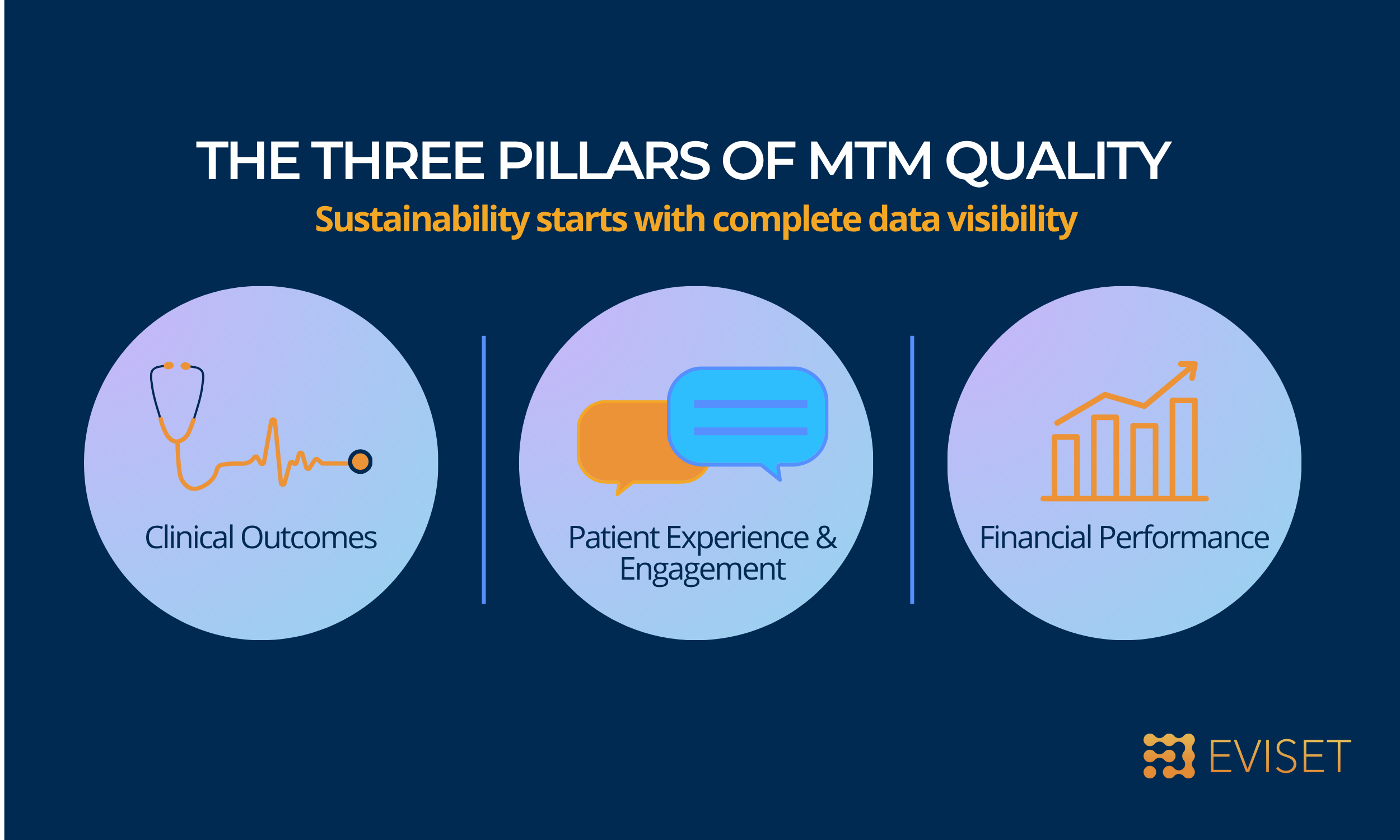
Finally, uniform standards across MTM providers will be essential to evaluate value consistently. These standards should include patient experience as a core quality domain alongside clinical and financial metrics. Integrating patient-generated data into MTM evaluation frameworks will create a more complete and credible evidence base to sustain long-term healthcare coverage for FIM interventions. These data can also be leveraged for continuous quality improvement by providing real-time insights and feedback that enable providers to refine services, respond to participant needs, and strengthen program effectiveness in a timely manner.
Eviset welcomes the opportunity to contribute to the next phase of this work by supporting MTM providers in strengthening data infrastructure and capturing patient-generated data as part of program and service evaluation frameworks. We are eager to contribute insights on how patient-generated data can strengthen quality improvement, accountability, and the long-term sustainability of MTM programs as a covered healthcare service.
Eviset is proud to participate alongside leading organizations shaping the future of Food Is Medicine. We look forward to continuing the dialogue as policymakers, providers, and payers work together to strengthen quality, sustainability, and measurable impact in this field.